Patient History/Diagnosis
A 57-year-old man with a history of hypercholesterolaemia and cigarette smoking presented to a district general hospital following 3 days of intermittent chest pain. His initial ECG showed inferior ST elevation and in view of ongoing pain he was transferred to a primary PCI centre for emergency angiography.
Procedure
After insertion of a 6F sheath (Glidesheath Slender, Terumo) in the right radial artery, a 0.038-inch wire was used but met with resistance soon after exiting the sheath. The wire was removed and a forearm angiogram was obtained (see Figure 1). This revealed a radial artery loop with a recurrent radial artery arising from the apex of the loop.
To minimise spasm and catheter exchange it was decided to use balloon-assisted tracking of a single-guide catheter. A 0.014-inch J-tipped wire was passed to the ascending aorta via the recurrent radial artery. A 2 x 15 mm compliant balloon was inserted into a 6F Ikari Left 4 guide catheter (IL4.0, Terumo) until approximately half the balloon was protruding from the tip of the catheter. The balloon was then inflated to 6 atm and loaded onto the back end of the 0.014-inch wire. Both the balloon and catheter were then passed with no resistance into the proximal ascending aorta. After withdrawal of the balloon and wire, coronary angiography was undertaken.
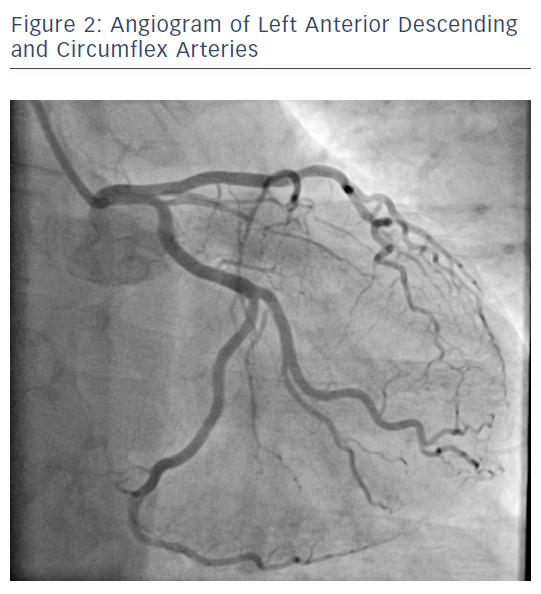
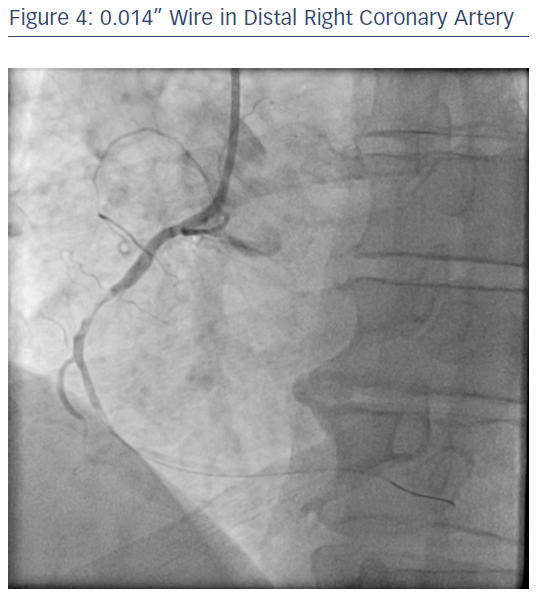
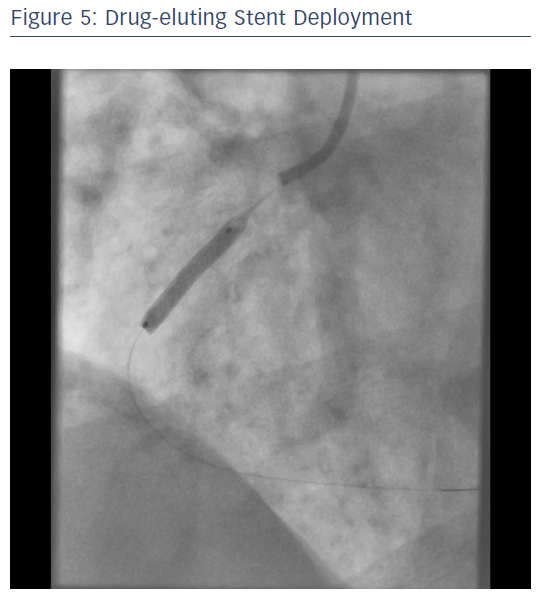
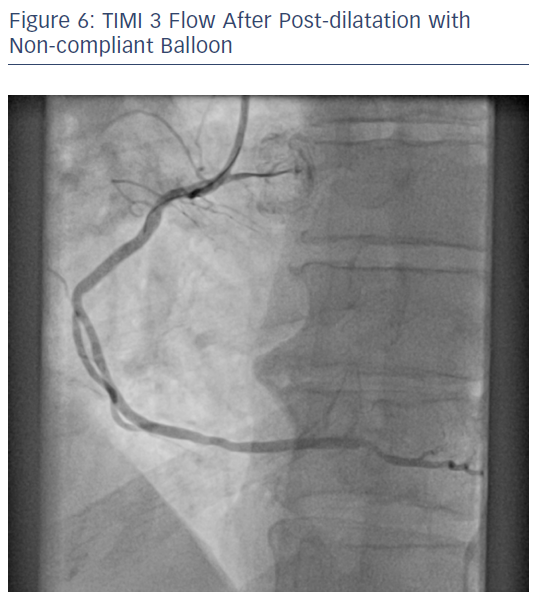
Angiography of the left coronary system revealed minor disease in the left anterior descending and circumflex (see Figure 2). The same catheter was used to engage the right coronary ostium revealing a proximal occlusion with TIMI 0 flow (see Figure 3). Passage of the 0.014-inch wire to the distal right coronary artery restored TIMI 2 flow (see Figure 4) and an aspiration catheter (Eliminate, Terumo) was then deployed. A residual proximal stenosis was then dilated with a 2 x 15 mm compliant balloon, following which, a 3 x 18 mm drug eluting stent (see Figure 5) was deployed and post dilated with a 3.5 x 8 mm non-compliant balloon resulting with TIMI 3 flow (see Figure 6).
Conclusion
Use of balloon-assisted tracking can minimise spasm and facilitate negotiation of difficult radial anatomy. Use of a single multipurpose guide catheter minimises the need for catheter exchanges and in the setting of primary percutaneous cardiac intervention can reduce the door-to-device time.
Comments
Abnormal radial anatomy is present in 14 % of patients. Radial loops are associated with higher risks of procedural failure. Early identification of abnormal radial anatomy allows for steps to be taken to minimise spasm and increase the chances of procedural success.