ACC 2022: Late-breaking Science Video Collection
Published: 05 April 2022
-
Views:
 7932
7932
-
Likes:
 7
7
-
Views:
 7932
7932
-
Likes:
 7
7
-
 Up Next
Up Next -
 10m 24s
10m 24s -
 3m 50sPart 3 | Session 18 ACC 22: 3-year Efficacy Outcomes from the SPYRAL HTN-ON MED Med Pilot Study
3m 50sPart 3 | Session 18 ACC 22: 3-year Efficacy Outcomes from the SPYRAL HTN-ON MED Med Pilot Study -
 4mPart 3 | Session 19 2022 AHA/ACC/HFSA Guideline for HF Management: Highlights & Implementation
4mPart 3 | Session 19 2022 AHA/ACC/HFSA Guideline for HF Management: Highlights & Implementation
-
 12m 6sPart 4 | Session 1 ACC 22: 3 Trials That Will Change Your Practice with Dr Purvi Parwani
12m 6sPart 4 | Session 1 ACC 22: 3 Trials That Will Change Your Practice with Dr Purvi Parwani -
 6m 15s
6m 15s -
 7m 9sPart 4 | Session 3 4 Lipid Late-breaker Highlights from ACC.22 with Dr Erin Michos
7m 9sPart 4 | Session 3 4 Lipid Late-breaker Highlights from ACC.22 with Dr Erin Michos
-
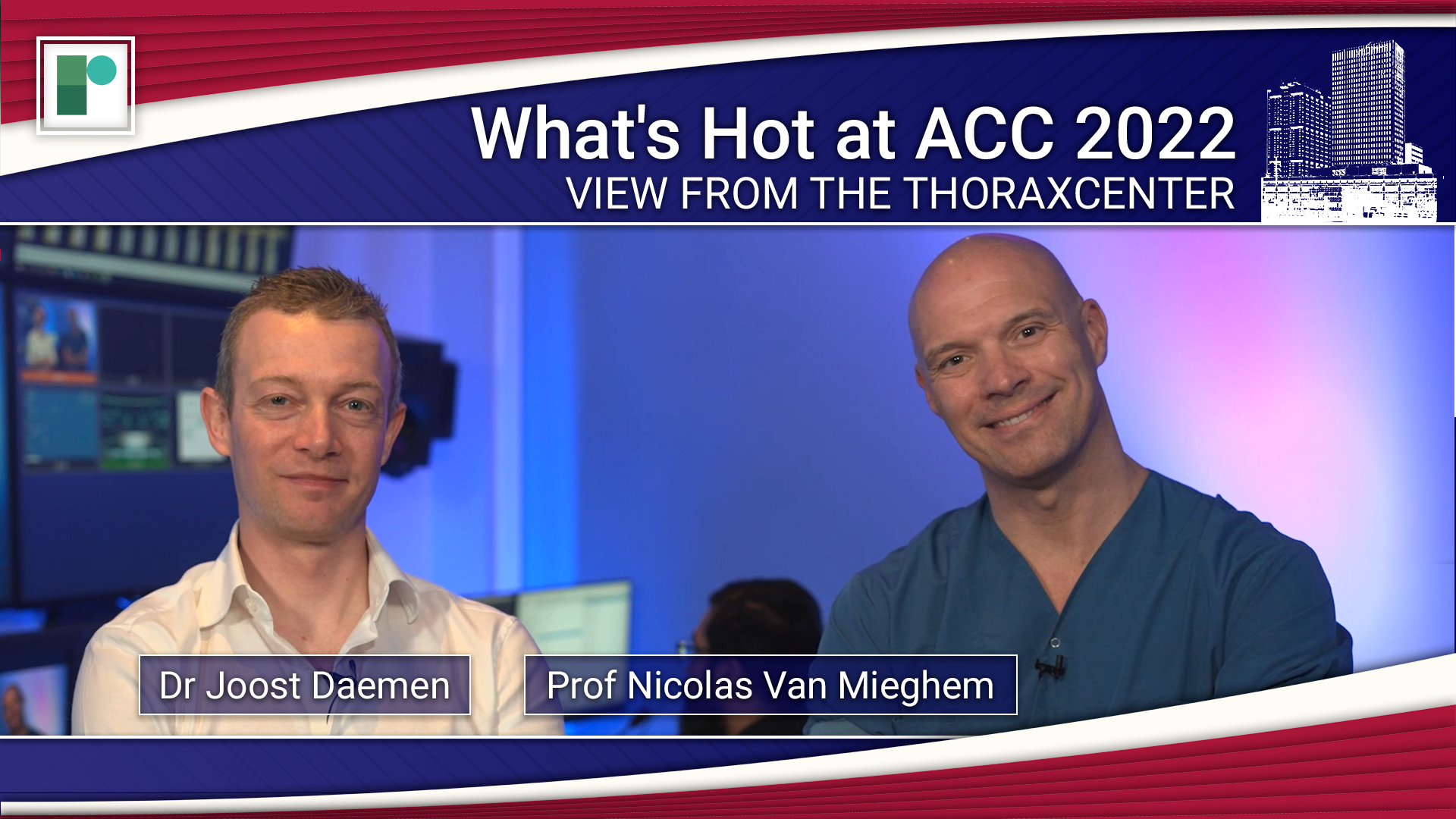 23m 9sPart 1 | Session 1 ACC 22 Late-breaking Science Preview Nicolas M Van Mieghem, Joost Daemen
23m 9sPart 1 | Session 1 ACC 22 Late-breaking Science Preview Nicolas M Van Mieghem, Joost Daemen
-
 28m 6sPart 1 | Session 2 ACC.22 Late-breaking Science Wrap-Up Nicolas M Van Mieghem, Joost Daemen
28m 6sPart 1 | Session 2 ACC.22 Late-breaking Science Wrap-Up Nicolas M Van Mieghem, Joost Daemen
-
 16m 42sPart 2 | Session 1 ACC 2022 Late-breaker Discussion: The SODIUM-HF Trial Justin Ezekowitz, Harriette Van Spall
16m 42sPart 2 | Session 1 ACC 2022 Late-breaker Discussion: The SODIUM-HF Trial Justin Ezekowitz, Harriette Van Spall
-
 16m 57sPart 2 | Session 2 ACC 2022 Late-breaker Discussion: The SuperWIN Trial Harriette Van Spall, Dylan L Steen
16m 57sPart 2 | Session 2 ACC 2022 Late-breaker Discussion: The SuperWIN Trial Harriette Van Spall, Dylan L Steen
-
 15m 38sPart 2 | Session 3 ACC 22 Late-breaker Discussion: The PROMPT-HF Trial Harriette Van Spall, Gregg C Fonarow, Tariq Ahmad
15m 38sPart 2 | Session 3 ACC 22 Late-breaker Discussion: The PROMPT-HF Trial Harriette Van Spall, Gregg C Fonarow, Tariq Ahmad
-
 22m 47sPart 2 | Session 4 ACC 22 Late-breaker Discussion: The DIAMOND Trial Harriette Van Spall, Javed Butler, Faiez Zannad
22m 47sPart 2 | Session 4 ACC 22 Late-breaker Discussion: The DIAMOND Trial Harriette Van Spall, Javed Butler, Faiez Zannad
-
 9m 38sPart 3 | Session 1 ACC 22: Findings from the VALOR-HCM Trial Milind Y Desai
9m 38sPart 3 | Session 1 ACC 22: Findings from the VALOR-HCM Trial Milind Y Desai
-
 7m 19sPart 3 | Session 2 ACC 22: MAVA-LTE Shows Improvement in NYHA Class in Patients Treated with Mavacamten Florian Rader
7m 19sPart 3 | Session 2 ACC 22: MAVA-LTE Shows Improvement in NYHA Class in Patients Treated with Mavacamten Florian Rader
-
 3m 19sPart 3 | Session 3 ACC 22: Results From the PACIFIC AF Trial Manesh R Patel
3m 19sPart 3 | Session 3 ACC 22: Results From the PACIFIC AF Trial Manesh R Patel
-
 3m 6sPart 3 | Session 4 ACC 22: FAME 3 Suggests CABG Outperforms FFR-Guided PCI in Patients with Multivessel Disease Frederik Zimmermann
3m 6sPart 3 | Session 4 ACC 22: FAME 3 Suggests CABG Outperforms FFR-Guided PCI in Patients with Multivessel Disease Frederik Zimmermann
-
 3m 54sPart 3 | Session 5 ACC 22: Results from the TRANSLATE-TIMI 70 Trial Brian Bergmark
3m 54sPart 3 | Session 5 ACC 22: Results from the TRANSLATE-TIMI 70 Trial Brian Bergmark
-
 4m 22sPart 3 | Session 6 ACC 22: Results from the POISE-3 Trial Philip J Devereaux
4m 22sPart 3 | Session 6 ACC 22: Results from the POISE-3 Trial Philip J Devereaux
-
 6m 30sPart 3 | Session 7 ACC 22: ICD Shock Therapies and the Burden of Ventricular Tachycardia Paolo Della Bella
6m 30sPart 3 | Session 7 ACC 22: ICD Shock Therapies and the Burden of Ventricular Tachycardia Paolo Della Bella
-
 6m 3sPart 3 | Session 8 ACC 22: PACMAN-AMI Shows Reduced Plaque Regression in AMI Patients Treated with Alirocumab Lorenz Räber
6m 3sPart 3 | Session 8 ACC 22: PACMAN-AMI Shows Reduced Plaque Regression in AMI Patients Treated with Alirocumab Lorenz Räber
-
 3m 31sPart 3 | Session 9 ACC 22: Magnitude & Duration of Effects of a siRNA Targeting Lp(a) Steven E Nissen
3m 31sPart 3 | Session 9 ACC 22: Magnitude & Duration of Effects of a siRNA Targeting Lp(a) Steven E Nissen
-
 4m 48sPart 3 | Session 10 ACC 22: Results From a sub-study of the POISE-3 Trial Maura Marcucci
4m 48sPart 3 | Session 10 ACC 22: Results From a sub-study of the POISE-3 Trial Maura Marcucci
-
 2m 55sPart 3 | Session 11 ACC 22: Findings from the CoreValve US Pivotal & SURTAVI Trials Michael J Reardon
2m 55sPart 3 | Session 11 ACC 22: Findings from the CoreValve US Pivotal & SURTAVI Trials Michael J Reardon
-
 7m 44sPart 3 | Session 12 ACC 22: ADAPT-TAVR Shows SLT Does Not Affect CO for Patients After TAVR Duk-Woo Park
7m 44sPart 3 | Session 12 ACC 22: ADAPT-TAVR Shows SLT Does Not Affect CO for Patients After TAVR Duk-Woo Park
-
 5m 41sPart 3 | Session 13 ACC 22: Results From the Chocolate-Touch Study
5m 41sPart 3 | Session 13 ACC 22: Results From the Chocolate-Touch Study
-
 2m 25sPart 3 | Session 14 ACC 22: Results from the GIPS-IV Trial Pim van der Harst, Marie-Sophie de Koning
2m 25sPart 3 | Session 14 ACC 22: Results from the GIPS-IV Trial Pim van der Harst, Marie-Sophie de Koning
-
 9m 27sPart 3 | Session 15 ACC 22: FFR vs. IVUS-guided PCI in Intermediate Coronary Artery Stenosis: The FLAVOUR Trial Bon-Kwon Koo
9m 27sPart 3 | Session 15 ACC 22: FFR vs. IVUS-guided PCI in Intermediate Coronary Artery Stenosis: The FLAVOUR Trial Bon-Kwon Koo
Overview
Our regular review series View from the Thoraxcenter hosted by Prof Nicolas Van Mieghem and Dr Joost Daemen (Thoraxcentre, Erasmus MC, Rotterdam, NL) provide a concise analysis of the late-breaking science results and spotlight impactful data.
For a deeper dive into key clinical trial data, Dr Harriette Van Spall (McMaster University, Hamilton, CA)talks with principal investigators in her regular Late-Breaker Discussion Series.
Short, accessible Expert Interviews were conducted with select faculty focusing on the results, applicability, and impact on future research.
More from this programme
Part 1
View from the Thoraxcenter
Part 2
Late-breaker Discussion Series
Part 3
Expert Interviews
Faculty Biographies
Mikhail Kosiborod
Cardiologist
Dr Mikhail Kosiborod is a cardiologist, the Vice President of Research at Saint Luke's Health System, and Professor of Medicine at the University of Missouri-Kansas City, US.
He is also Director of Cardiometabolic Research and Co-Director of the Saint Luke’s Michael & Marlys Haverty Cardiometabolic Center of Excellence at Saint Luke's Mid America Heart Institute. Dr Kosiborod is an internationally-recognised expert in the fields of diabetes and cardiovascular disease, cardiometabolic and cardiorenal syndromes.
Dr Kosiborod is involved in the leadership of numerous clinical trials and multi-center registries, and is currently the principal investigator of several investigator-initiated, multi-center trials in diabetes and cardiovascular disease.
Transcript
Study Rationale
In this analysis of EMPULSE trial, we looked at the effects of empagliflozin SGLT2 inhibitor, on health status which is symptoms, physical limitations, and quality of life in patients hospitalised with acute heart failure. Just to take a step back, we presented the main result of EMPULSE at the American heart association a few months ago and it was just published recently. And it is important to keep in mind that patients hospitalised with acute heart failure experience, very high burden of symptoms in physical limitations and poor quality of life. And we have a depth of therapies that can be effective in improving those outcomes. In the main EMPULSE study, we previously showed that empagliflozin is compared with placebo significantly improved, what we call total clinical benefit which is a composite theoretical, composite of death recurrent heart failure events, and change in Kansas city cardiomyopathy questionnaire, which is a measure of symptoms, physical limitations, and quality of life. But in this analysis specifically, we wanted to concentrate on the effects of empagliflozin on those very outcomes, very important outcomes to patients with acute heart failure, which is the symptom burdens a burden of physical limitations and the poor quality of life.
Study Design and Patient Population
EMPULSE trial enrolled over 500 patients as it were hospitalised with acute heart failure. It's really a unique trial in many ways, because it included patients with acute heart failure regardless of the ejection fraction. So, both those reduced the preserved ejection fraction, were enrolled as well as those with or without diabetes. And also those with either worsening chronic heart failure or De novo heart failure. Which means that was a new diagnosis of acute heart failure patients were hospitalised with. So all of those types of patients were included in the study and while on hospitals they were randomised to either empagliflozin or placebo and treated for 90 days. Specifically for the outcomes that we concentrated on in this analysis, Kansas city cardiomyopathy questionnaire which is a gold standard of health status that was assessed at randomization as well as 15, 30 and 90 days.
Main Findings
So in this particular and analysis there were two key objectives. One is to evaluate the effective empagliflozin on the primary endpoint which was a total clinical benefit, across the totals of Kansas City cardiomyopathy questionnaire scores. So, essentially to try to understand whether this is a clinical total clinical benefit of empagliflozin different, depending on degree of symptomatic impairment of baseline. And second, perhaps even more importantly to look at the effect of empagliflozin on symptoms, physical limitations of quality of life during the treatment period. So, you know, what happens after 15, 30 and 90 days of treatment? So in terms of what we found for the first objective. We, saw that empagliflozin as compared with placebo, significantly benefit patients in terms of a total clinical benefit to against that hierarchical composite of death, heart flow events and change in Kansas City cardiomyopathy questionnaire to a similar extent, regardless of the degree of symptomatic impairment at baseline. And for the second objective, we found that patients treated with empagliflozin had significantly greater improvement in the symptoms, as well as physical limitations and quality of life over time. And importantly, that benefit emerged already at 15 days and was sustained up to 90 days. So very, very quick onset of benefit and then consistent benefit over time.
Recommendations for Use
Right, So, as I mentioned earlier, we have durable treatments in acute heart failure that have been proven to significantly improve symptoms, physical limitations, quality of life, in those patient populations that's really symptomatically and functionally impaired. And I think the message from this data is that SGLT2 inhibition for patients acutely hospitalised with heart failure is a treatment that won't just potentially improves clinical events. But also make patients feel better and enable them to be able to do more. Which is a critical goal of care in this patient population. So yet another very important incentive to potentially think about initiating SLGT2 inhibitors in the hospital, in patients with heart failure regardless of what type of heart failures they have whether it's reduced or preserved ejection fraction. Whether it is chronic decompensated or de novo heart failure. Because we thought that the results on health status were very consistent across all of those subgroups.
Further Research Required
Well, I think we already have a lot of data on SGLT2 inhibition and heart failure, all different types of heart failure. But, in the acute heart failure space there is more data coming. I think importantly. So there are ongoing studies looking at dapagliflozin in acute decompensated, heart failure. I think that will further better the evidence base. And then also very importantly, we also have in heart failure with preserved ejection fraction, a second large outcome trial with dapagliflozin, DELIVER which will be the largest trial of patients with HFpEF with the longest duration of follow up. So, really will help hopefully solidify the evidence base for patients with heart failure and preserve them which is really need of additional therapies.





