What is atrial fibrillation?
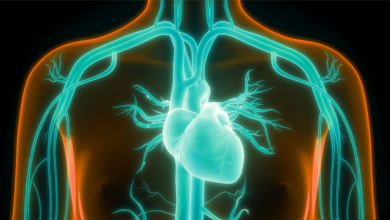
Atrial fibrillation (AF) is the most common sustained type of cardiac arrhythmia, characterised by irregularly irregular ventricular pulse and loss of association between the cardiac apex beat and radial pulsation.
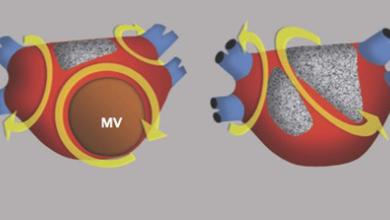
With atrial fibrillation, the irregular heartbeat is often very rapid, which can result in blood clots in the heart, strokes and other heart related issues so should be treated as a serious medical issue which needs to be addressed. The atrias (upper chambers) beat chaotically and out of sync with the ventricles (lower chambers) and may cause heart palpitations, shortness of breath and weakness.
Symptoms of atrial fibrillation
Atrial fibrillation causes an irregular heartbeat which is often abnormally fast, in some cases being considerably higher than 100 beats per minute. This can often lead to other symptoms such as dizziness, shortness of breath or tiredness.
With atrial fibrillation, heart palpitations will often be noticeable where the heart will often feel like it is pounding hard, fluttering or beating irregularly. These can last either a few seconds or a few minutes. Other symptoms include chest pain, fatigue or finding it difficult to exercise. Other times, atrial fibrillation may have no noticeable symptoms at all.
Atrial fibrillation might be permanent, or may come and go, which is known as paroxysmal atrial fibrillation.
What causes atrial fibrillation?
The most common cause of atrial fibrillation is damage to the heart’s structure. This damage can be caused by any of the following:
- Heart disease (heart valve disease, congenital heart disease, coronary heart disease)
- High blood pressure
- Obesity
- Lifestyle (alcohol, smoking)
- Pericarditis
- Cardiomyopathy
- Diabetes
- Heart surgery
- Stress
- Sick sinus syndrome
- Sleep apnoea
Diagnosing atrial fibrillation
AF may be paroxysmal, persistent or permanent. Diagnostic investigation typically includes a complete history, physical examination, ECG, transthoracic echocardiogram, full blood count and serum thyroid-stimulating hormone level.
- Complete history: A complete history and risk stratification of the patient should be conducted to get a better understanding of the severity of the atrial fibrillation. The history should focus on symptoms such as chest pain, shortness of breath, palpitations, dizziness, increased lower extremity swelling and dyspnea on exertion as well as wider issues such as heart disease.
- Physical examination: A full physical exam should be conducted to try and identify the cause of atrial fibrillation. This may include checking the neck for signs of thyroid, pulmonary examination, cardiovascular exam, abdominal exam and an exam of the central nervous system.
- Atrial fibrillation ECG: An ECG will measure the patient's heart rate and record any abnormalities with the heart rate, such as the typical ‘irregularly irregular’ pattern.
- Transthoracic echocardiogram: This ultrasound scan looks at the heart and nearby blood vessels to better understand their structure, blood flow and the condition of the heart chambers.
- Full blood count: Lab work will help to identify any causes of AF, such as infections or heart damage.
- Serum thyroid stimulating hormone level: Testing whether any issues with the thyroid are contributing to the atrial fibrillation.
Atrial Fibrillation treatment
Management involves control of the arrhythmia (by rhythm or rate control) and thromboprophylaxis to prevent strokes. Any underlying cause, such as acute infection or hyperthyroidism needs to be treated.
Options for treating AF include lifestyle changes, medication, medical procedures and surgery. The choice of treatment is based on heart rate and symptoms. Rate control is the first-line strategy. When medications are not effective, a procedure may be necessary – electrical cardioversion, pulmonary vein isolation ablation, catheter ablation of the AV node with a pacemaker or device therapy.
- Lifestyle changes: Increasing exercise frequency, avoiding smoking or drinking alcohol and caffeine, eating a nutritious diet and managing stress.
- Medication: Medication such as beta blockers and calcium channel blockers may be used to reduce the heart rate.
- Medical procedures: Cardioversion, where the heart is given an electric shock to try and restore normal rhythm.
- Surgery: Catheter ablation, where radiofrequency energy is used to destroy any areas of the heart causing the atrial fibrillation. A pacemaker may then be fitted.