The Treatment of Bifurcation Disease is a challenging area in interventional cardiology. It presents a challenge as interventional cardiology takes on increasingly complex coronary cases.
Studies report that when compared to non-bifurcation stenting, intervention to bifurcation disease is associated with lower rates of success, higher costs, longer hospitalisation and a higher rate of clinical and angiographic restenosis. Whilst the use of drug-eluting stents (DESs) has improved some outcomes, side branch ostial residual stenosis and long-term restenosis remain a problem.
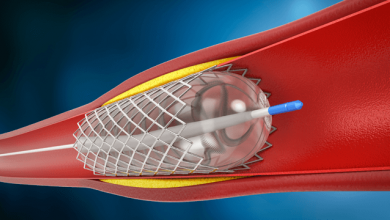
Bifurcation stenting requires a diverse armamentarium of stenting strategies. Provisional stenting to the main vessel, tackling the side branch only if there is a poor angiographic result remains the prevailing approach. Other more complex two stent approaches include those that stent the main branch first, such as elective T-Stenting, the Culotte and TAP approaches. Other approaches include those that stent the side-branch first such as the various Crush approaches. Innovations such as dedicated bifurcation stents and improved stent and balloon technologies will mean bifurcation approaches will expand and evolve rapidly.
With so many different approaches, it can be seen that the most important question in bifurcation disease PCI is selecting the best possible strategy for an individual bifurcation and optimising the performance of this technique. Educating Interventional Cardiologists will be essential to keep up-to-date on the current data and help physicians choose the most relevant procedure for their patient.