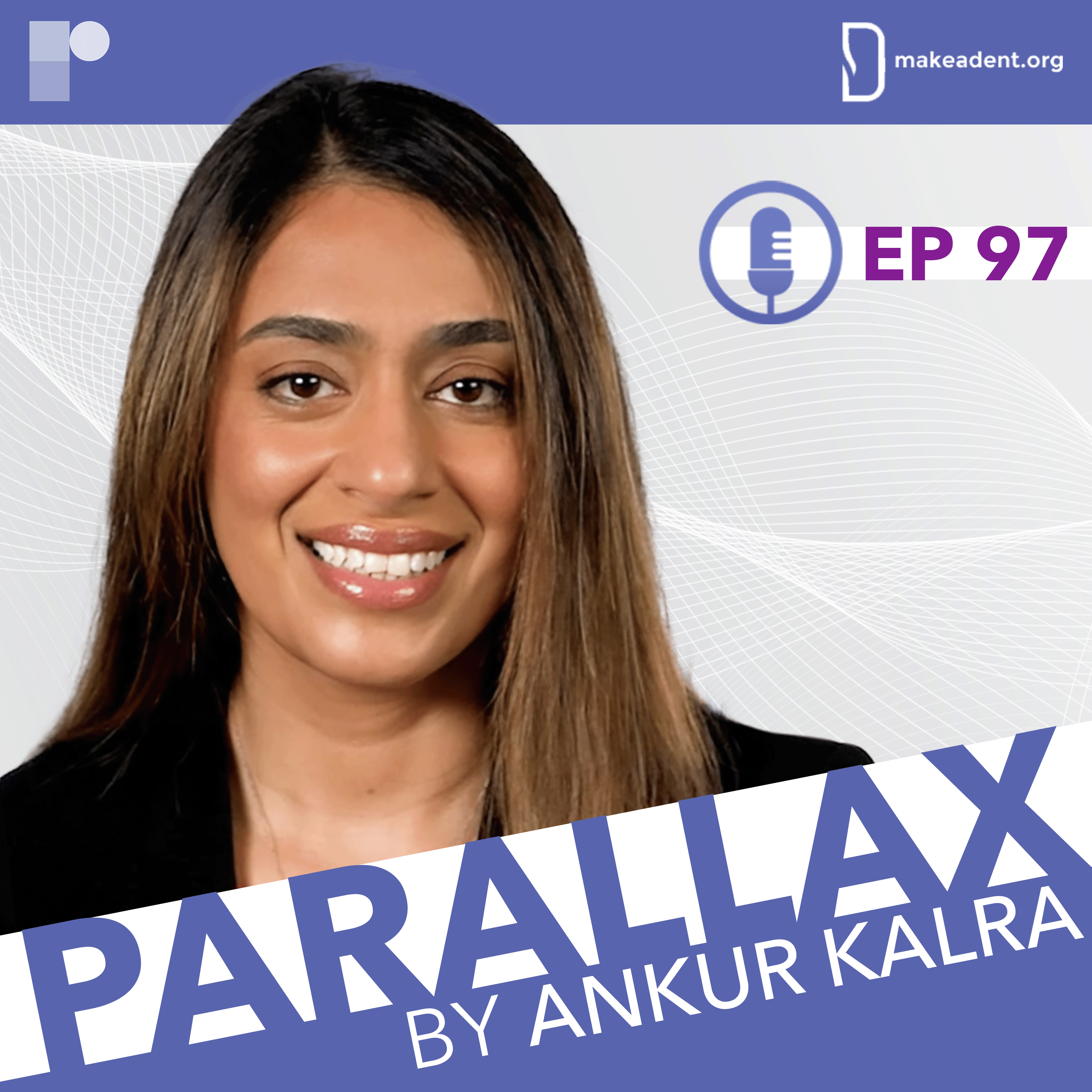
In the finale of our series "Conversations about Hypertrophic Cardiomyopathy", Dr Ankur Kalra welcomes, Dr Anjali Tiku Owens, for a dynamic and practical discussion.
Dr Owens is Medical Director of the Center for Inherited Cardiac Disease and Associate Professor of Medicine at the Hospital of the University of Pennsylvania.
This series is supported by an unrestricted educational grant from Bristol Myers Squibb. Please see www.camzyosrems.com for important safety information.
In this week’s episode, Dr Kalra and Dr Owens take us on a journey through the complexities of hypertrophic cardiomyopathy (HCM), with focus on the diagnostic challenges and breakthroughs in this field.
Emphasising with the critical importance of making accurate diagnoses, Dr Owens shares her insights into identifying the common mimickers of HCM through a structured approach starting with taking the patients history.
As the conversation delves deeper, Dr Owens discusses the various diagnostic tools and tests used to rule out other conditions and uncover the underlying aetiology. She navigates us through the algorithm for interpreting genetic test results, differentiating pathogenic variants, benign variants and variants of uncertain significance (VUS). Dr Owens talks about the wider implications for family members and the cases in which she recommends screening.
Dr Kalra asks Dr Owens about her approach to exercise in HCM patients. Additionally, they cover the debated topic of defibrillator therapy and the use of HCM Risk-SCD risk calculator.
Dr Owens provides an overview of the treatment paradigms for HCM, touching on haemodynamic classifications, symptomatology and the evaluation of sudden death risk.
What are the most common mimickers of HCM? What is Dr Owens and her heart team approach to decision making? What is the role of genetic testing in patients with HCM?
This content is intended for US-based physicians.
This series is supported by an unrestricted educational grant from Bristol Myers Squibb.

As we adapt to the changes brought about by the pandemic, Dr Singh outlines the necessary steps to foster a reality in which we can utilize these technologies to create more time for human connection.





Dr Gerdisch shares insights into his research on rigid sternal fixation and enhanced recovery protocols, which have shown promising results in postoperative pain management and patient recovery.


Parallax’s guest this week is Dr Eric David Adler, Medical director of heart transplant and mechanical circulatory support at UC San Diego Health.

How did Dr Gragossian receive her diagnosis? How does she feel about her new reality? What drives her? What is her message to our listeners?

Just after 9/11, Heval, the 18-year-old Syrian Kurdish refugee found a job as a dishwasher. At this point, he was the sole provider of his family. The pressure that comes from being poor did not leave him for many years. Today, he is firm believer in giving back to underserved communities by spreading awareness within the medical community. As he says, well-meaning people of privilege are sometimes afraid to act. What we need is more people to bridge the gap and find ways to help each other.

What drives Dr Nishtha Sodhi? What were the formative moments of Dr Sodhi’s career? What are the new frontiers of cardiology?






