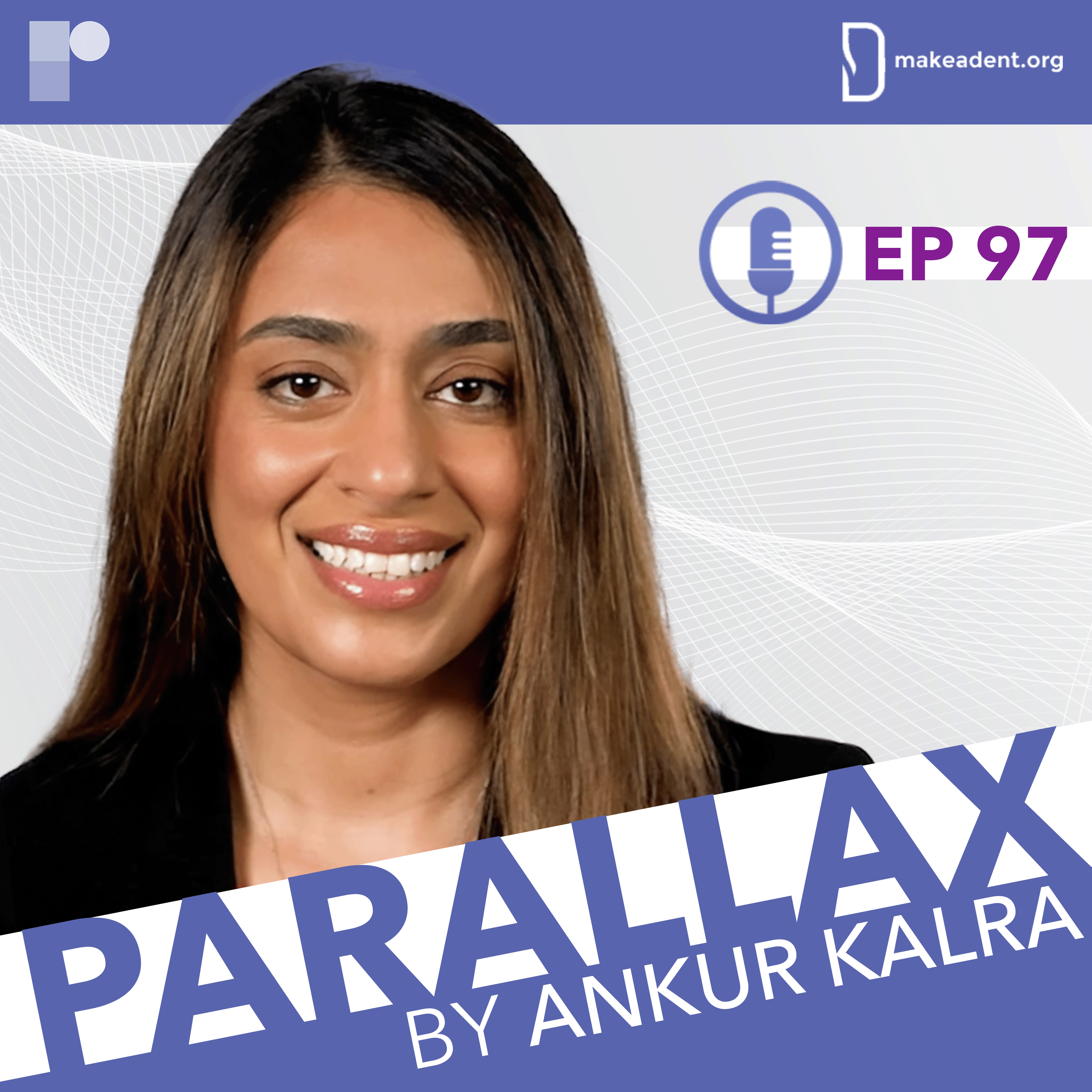
In the finale of our series "Conversations about Hypertrophic Cardiomyopathy", Dr Ankur Kalra welcomes, Dr Anjali Tiku Owens, for a dynamic and practical discussion.
Dr Owens is Medical Director of the Center for Inherited Cardiac Disease and Associate Professor of Medicine at the Hospital of the University of Pennsylvania.
This series is supported by an unrestricted educational grant from Bristol Myers Squibb. Please see www.camzyosrems.com for important safety information.
In this week’s episode, Dr Kalra and Dr Owens take us on a journey through the complexities of hypertrophic cardiomyopathy (HCM), with focus on the diagnostic challenges and breakthroughs in this field.
Emphasising with the critical importance of making accurate diagnoses, Dr Owens shares her insights into identifying the common mimickers of HCM through a structured approach starting with taking the patients history.
As the conversation delves deeper, Dr Owens discusses the various diagnostic tools and tests used to rule out other conditions and uncover the underlying aetiology. She navigates us through the algorithm for interpreting genetic test results, differentiating pathogenic variants, benign variants and variants of uncertain significance (VUS). Dr Owens talks about the wider implications for family members and the cases in which she recommends screening.
Dr Kalra asks Dr Owens about her approach to exercise in HCM patients. Additionally, they cover the debated topic of defibrillator therapy and the use of HCM Risk-SCD risk calculator.
Dr Owens provides an overview of the treatment paradigms for HCM, touching on haemodynamic classifications, symptomatology and the evaluation of sudden death risk.
What are the most common mimickers of HCM? What is Dr Owens and her heart team approach to decision making? What is the role of genetic testing in patients with HCM?
This content is intended for US-based physicians.
This series is supported by an unrestricted educational grant from Bristol Myers Squibb.

As we adapt to the changes brought about by the pandemic, Dr Singh outlines the necessary steps to foster a reality in which we can utilize these technologies to create more time for human connection.


In this episode, Ankur and Danielle speak about the evidence in favour of a whole-food plant-based diet to improve cardiovascular health, the ACC prevention guidelines, how to talk to patients about positive dietary change, the issue of lack of nutrition training in cardiovascular fellowships and what Danielle’s diet looks like as a busy whole-food plant-based cardiology fellow. On her own podcast ‘Nutrition Rounds’ Danielle has discussions about evidence-based plant-based nutrition with physicians who are leading experts in nutrition and health.
Hosted by @AnkurKalraMD. Produced by @RadcliffeCardiology.
In this brilliant conversation, Ankur, Emmanouil and Michael unravel the potential advantages, challenges and practical realities of using drug-coated balloons in SVD, and the findings of the latest randomised controlled trials studying this area.
Hosted by @AnkurKalraMD. Produced by @RadcliffeCardiology. [Disclaimer: The use of drug-coated balloons in coronay intervention is still off-label; it has not been approved by the FDA.]

Dawn is an associate editor of the journal Circulation: Cardiovascular Interventions and is widely known for her research program on PCI and peripheral arterial disease (PAD). Ankur and J. Dawn discuss multiple trials/studies that were published in 2018, including ORBITA, PIONEER-II and ABSORB. J. Dawn also shares her thoughts on the latest stent technologies.
Hosted by @AnkurKalraMD. Produced by @RadcliffeCardiology.
They discuss the importance of preventative medicine, their experience of reducing hypertension with non-pharmaceutical and pharmaceutical methods, and the significance of the integrated “team approach” when treating comorbid conditions such as hypertension. Athena also shares her thoughts on cardiologists’ responsibility to shape their patients’ lifestyle choices.
Hosted by @AnkurKalraMD. Produced by @RadcliffeCardiology.
Chest pain is one of the most common reasons for an emergency room visit in the US, with almost 6 million ER visits annually, yet there is no consensus on how to compare the results from various hscTn assays. Tune in to hear Santiago outline the advantages and limitations of using hscTn as a standard biomarket to evaluate patients with suspected ACS in the ER.
Hosted by @AnkurKalraMD. Produced by @RadcliffeCardiology.





